
February. What comes to mind? Ground Hog’s Day? Leap Year? Your brother-in-law’s birthday? Valentine’s Day?
I think about all of these and I am also reminded that this is the month where the medical community brings awareness to heart health. During this month, I will be taking time to talk to you about your heart health.
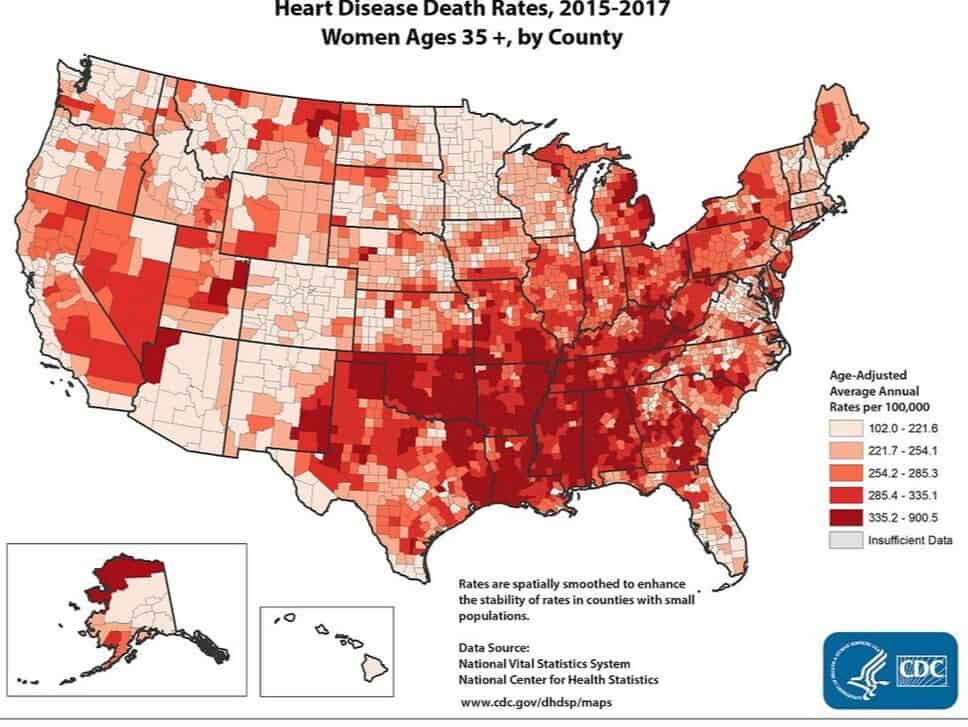
Did you know that cardiovascular disease is the leading cause of death in women, killing more women in the United States than all types of cancer combined? The latest statistics according to the CDC report 290,000 women died of heart disease versus 277,000 for all types of cancer in 2015-the latest numbers available. I know a lot of women who are scared that they will get a cancer diagnosis and give very little thought to their cardiovascular health.
For Information on Heart Disease in Women Visit the CDC
So, let’s talk about the difference between cardiovascular disease, heart disease, and coronary heart disease. Yes, they all sound similar, but there are some differences.
Here we go:
Cardiovascular disease is the term for all types of diseases that affect the heart or blood vessels which can cause heart attacks, stroke, congenital heart defects and peripheral artery disease.
Heart disease is a catch-all phrase for a variety of conditions that affect the heart’s structure and function. Keep in mind — all heart diseases are cardiovascular diseases, but not all cardiovascular diseases are heart disease. The most common type of heart disease is coronary heart disease. In fact, when people talk about “heart disease” they often mean coronary heart disease.
How do we develop cardiovascular diseases?
Trouble begins when excess cholesterol—carried through the bloodstream in protein-coated particles known as LDL, or “bad” cholesterol—builds up in artery walls. In a perfect world, you would have sufficient HDL, or “good” cholesterol particles, to sop up the excess and carry it to the liver for disposal. But many women do not have enough HDL. The immune system sees the cholesterol that remains in vessel walls as an invader and launches an inflammatory attack. White blood cells gobble up the cholesterol, becoming engorged with fat and mired in the vessel walls, where many of them die, spilling their contents. In an attempt to isolate the damage, the immune system then encases the area in a fibrous coat, forming atherosclerotic plaque better known as a clog or clot. But because the cholesterol hasn’t been eliminated, the inflammatory process persists.
When it happens in the heart and you have coronary artery disease, the plaque reduces the amount of oxygen-rich blood getting to your heart, which can cause chest pain (also called angina—which is a classic sign of a heart attack in men but not so much in women!). Plaque can also lead to blood clots, which block blood flow and are the most common cause of a heart attack.
There is a third way to develop heart attacks that is more common in women than men. It involves a condition known as coronary microvascular disease. The problem develops first in the smaller arteries of the heart that branch off the larger one. Instead of developing clots that burrow into the artery’s wall or poke out into the tube of the artery where the blood is flowing, these smaller vessels develop inflammation that narrows and stiffens them. They can’t open up when the body needs more blood flowing, so the heart doesn’t get all the blood it needs. Also the inflammation can lead to spasms that further reduce the blood flow to the heart causing symptoms of fatigue, diffuse of vague chest discomfort, shortness of breath, and sometimes heart attacks.
How are we tested is coronary artery disease is suspected?
Unfortunately, there are no good tests for detecting microvascular disease (yes, this is not good for women) since the standard tests were designed for detecting problems in large vessels. People with symptoms such as chest pain first have a noninvasive stress test to determine whether the heart is getting enough blood as oxygen demands increase. If these tests indicate reduced blood flow to the heart, the next step is coronary angiography—an x-ray that shows where the vessel is blocked and the size of the obstruction. Once pinpointed, the blockage may be flattened during coronary angioplasty or bypassed with a vessel graft. However, as many as 30% of women with angina have “clear” angiograms! But still have microvascular disease. Unfortunately, many women say their physicians never talk to them about coronary risk and sometimes don't even recognize the symptoms, mistaking them instead for signs of panic disorder, stress, and even hypochondria. Below is a great table so that you can educate yourself about the signs and symptoms!
Top Heart Attack Symptoms in Women
One Month Before a Heart Attack | During a Heart Attack |
Unusal Fatigue (71%) | Shortness of Breath (58%) |
Sleep Disturbance (48%) | Weakness (55%) |
Shortness of Breath (42%) | Unusal Fatigue (43%) |
Indigestion (39%) | Cold Sweat (39%) |
Anxiety (36%) | Dizziness (39%) |
Racing Heart (27%) | Nausea (36%) |
Weak/Heavy Arms (25%) | Weak/Heavy Arms (35%) |
Source: Circulation 2003, Vol. 108, p. 2621.
Are You at Risk?
Menopause and blood lipids (fatty acid). Before menopause, a woman's own estrogen helps protect her from heart disease by increasing HDL (good) cholesterol and decreasing LDL (bad) cholesterol. After menopause, women have higher concentrations of total cholesterol than men do. But this alone doesn't explain the sudden rise in heart disease risk after menopause. Elevated triglycerides are an important contributor to cardiovascular risk in women. Low HDL and high triglycerides appear to be the only factors that increase the risk of death from heart disease in women over age 65.
Diabetes. Diabetes increases the risk of heart disease in women more than it does in men, perhaps because women with diabetes more often have added risk factors, such as obesity, hypertension, and high cholesterol. Although women usually develop heart disease about 10 years later than men, diabetes erases that advantage. In women who've already had a heart attack, diabetes doubles the risk for a second heart attack and increases the risk for heart failure.
Smoking. Women who smoke are more likely to have a heart attack as male smokers. Women are also less likely to succeed in quitting, and women who do quit are more likely to start again. Moreover, women may not find nicotine replacement as effective, and — because the menstrual cycle affects tobacco withdrawal symptoms — they may get inconsistent results with antismoking medications.
Metabolic syndrome. This is a group of health risks — large waist size, elevated blood pressure, glucose intolerance, low HDL cholesterol, and high triglycerides — that increases your chance of developing heart disease, stroke, and diabetes. Harvard Medical School research suggests that, for women, metabolic syndrome is the most important risk factor for having heart attacks at an unusually early age.
Inflammation. Mounting evidence that inflammation is a major player in atherosclerosis has led researchers to develop a test for a marker of blood vessel inflammation. For years, doctors have measured blood levels of C-reactive protein (CRP), an indicator of inflammation, to monitor diseases such as pneumonia, rheumatoid arthritis, and lupus. However, a high-sensitivity test, called hsCRP, is more specific to blood vessels.
Studies show that people with the highest CRP levels are about twice as likely to develop coronary artery disease and suffer a heart attack or other cardiac event as people with the lowest levels. As a result, hsCRP test results are now increasingly used along with other markers (such as cholesterol and blood pressure) to estimate cardiovascular risk.
High blood pressure (hypertension). High blood pressure damages the cells lining arteries, prompting the immune system to mount an inflammatory response that contributes to the development of atherosclerotic plaques. These plaques cause the arteries to stiffen, which drives up blood pressure even more, setting up a vicious circle. If these plaques enlarge, rupture, or break off, they can also lead directly to heart attacks and strokes. The chance of developing complications increases with higher levels of blood pressure.
Throughout the rest of the month, we’ll be talking about the specifics of reducing your risk of cardiovascular disease.
The preview is:
Get Moving
Improve your diet
Improve your sleep hygiene and reduce your stress


