Have you been told you have a pelvic organ prolapse?
Let’s get to the bottom of it.
As you probably already know, the uterus (or womb as we call it in pregnancy) is located within the center of the pelvis, is pear-shaped, and is a critical organ of the female reproductive system.
The uterus and your bowel and bladder are all held in position by a group of muscles that lie between the pubic bone and tailbone inside the pelvis. We collectively refer to this hammock-like group of muscles as the “pelvic floor.”
Supported by connective tissue and ligaments, the pelvic floor muscles support the pelvic organs and your uterus to keep them in their proper place.
More Blogs From Nancy Branberg
How To Strengthen Your Pelvic Floor
Can Pelvic Organ Prolapse Cause Fatigue?
Is The Fear Of Covid-19 Stalling Your Path To Recovery?
However, if these connective tissues, muscles, and ligaments get weak or suffer damage, it causes the uterus to drop into the vagina – a condition we call uterine prolapse.
We also use pelvic organ prolapse to describe the same thing happening with the bowel, bladder, or top of the vagina.
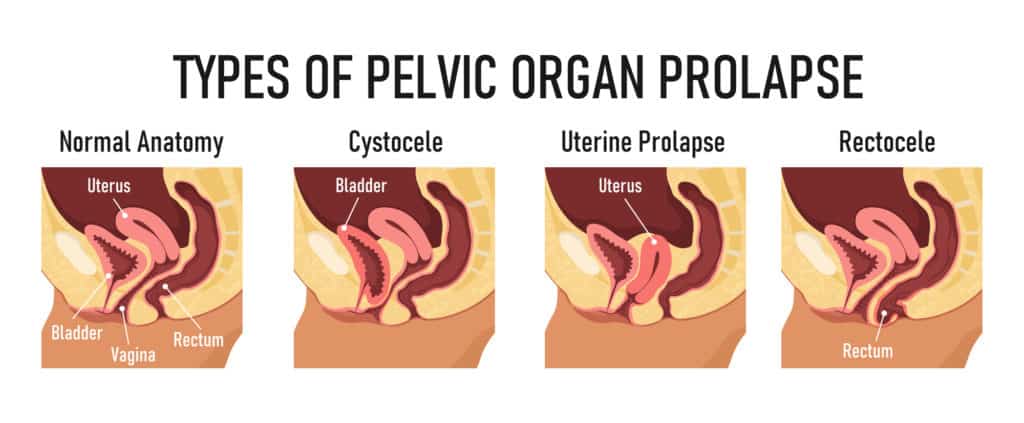
The main types of pelvic organ prolapse we see are:
- Anterior prolapse – where the bladder bulges into the vagina.
- Uterine prolapse – where the uterus drops into the vagina.
- Posterior wall prolapse – where the bowel protrudes into the rear wall of the vagina.
- Vaginal vault prolapse – where the top of the vagina sags and slips out of its normal position
However, it is also possible to have a pelvic organ prolapse that involves the small intestine or the urethra (the tube that runs from your bladder and out of the body), but these are less common.
The most common reasons for pelvic organ prolapse include pregnancy and natural childbirth, continuous coughing, menopause, or straining when visiting the toilet.
All of these can lead to damage to the pelvic floor muscles.
That’s why one of the best ways to treat and prevent pelvic organ prolapse is to learn how to perform pelvic floor exercises to strengthen weak muscles.
Another option, if the prolapse is severe, is to use a supportive pessary device to relieve the symptoms, which can be beneficial when combined with pelvic floor exercises.
In most cases, these two therapies combined are enough. Unfortunately, however, surgery may be required in severe cases – as an absolute last resort. But don’t worry; A specialist physical therapist can teach you how to strengthen your pelvic floor and help you avoid surgery altogether.
What Are The Signs And Symptoms Of Pelvic Organ Prolapse?
The symptoms of pelvic organ prolapse are wide and varied, but the most common symptoms we see include:
- A bulging sensation within the vagina
- Pressure and discomfort in the vagina
- Pain during sexual intercourse
- A heavy feeling in your lower abdomen
- A “dragging” or pulling sensation in or around your vagina
- Feeling like you’re sitting on something
- Seeing or touching a lump coming out of or inside your vagina
- Urinary stress incontinence, feeling like your bladder is still full after urinating, leakage, or needing to go to the bathroom more frequently.
What Are The Different Stages of Uterine Prolapse?
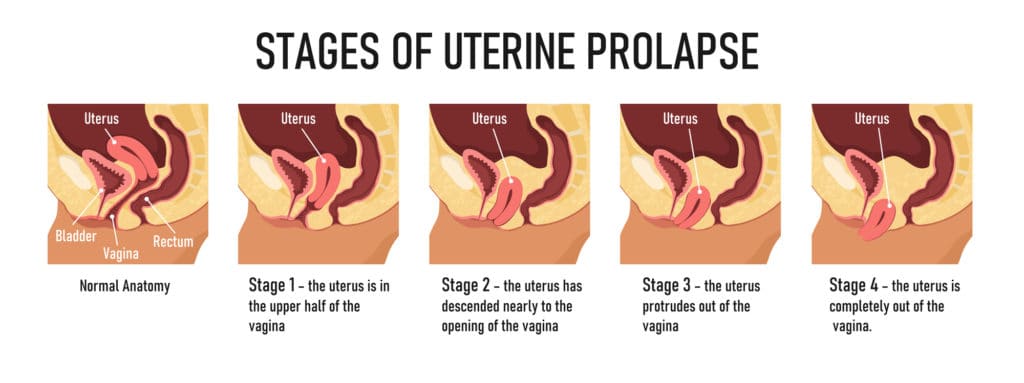
To help diagnose and treat your condition – speaking specifically about uterine prolapse – we use different categories to describe the condition divided into four stages:
- Stage One: The uterus bulges into the upper half of the vagina
- Stage Two: It hangs down near the opening of the vagina
- Stage Three: In this stage, the uterus protrudes out of the vagina
- Stage Four: It slips entirely outside the vagina
What Causes Pelvic Organ Prolapse?

The leading cause of pelvic organ prolapse is weak pelvic floor muscles, but what causes them to weaken in the first place?
It could be:
- Having multiple pregnancies or giving birth to more than one baby, as with twins/triplets and other multiple births.
- Excessive coughing due to asthma or bronchitis
- Severe exertion or straining when using the toilet to empty the bowels
- Uterine fibroids
- A tumor in the pelvic region (rarely)
- Lowered estrogen levels during the onset of menopause
How To Treat Pelvic Organ Prolapse

The treatment for uterine prolapse and other types of pelvic organ prolapse includes non-surgical and surgical options.
The most appropriate option for you is driven by your symptoms – with the guidance of a professional, like your doctor or a specialist women’s health physical therapist. But the treatment options include:
- Therapy to strengthen the pelvic floor
- Using a supportive vaginal pessary
- Opting for vaginal surgery
Treating Pelvic Organ Prolapse with Pelvic Floor Exercises
If you’re suffering from a Stage One uterine prolapse, you will find pelvic floor strengthening exercises particularly helpful. However, you need to do them correctly and preferably seek professional supervision from a pelvic floor physical therapist at the earliest available opportunity to prevent the condition from progressing to Stage Two and beyond. We have the experience and expertise to guide you through the movements to get the best possible results.
If necessary, you can do pelvic floor exercises or “Kegels” at home – although this is nowhere near as effective as professional therapy, and your progress will be slow. But to find your pelvic floor muscles:
- Place two fingers within your vagina and try squeezing them
- Contract the muscles within your anus as if you are trying to avoid gas
The muscles you tighten and grip when performing these exercises are your pelvic floor muscles. Once you’ve found them, you can start exercising and strengthening them by contracting and holding them repeatedly throughout the day.
You can do these exercises anytime, standing, sitting, or lying down. Try to do around six sessions daily while in the early stages of learning the exercises. But once you’ve got the hang of it and can do them correctly, just three sessions a day is adequate.
Remember: Always focus on your “pelvic floor” muscles before beginning the exercises. Relax your legs, abdominal, and butt muscles completely. Also, don’t hold your breath. Breath smoothly and deeply throughout the exercises.
Then squeeze and contract your vagina, urethra, and anus for 3 seconds before releasing. Repeat. When lifting weights, coughing, or sneezing, always squeeze and lift the pelvic floor muscles. Feeling the abdomen tighten quite gently while performing the exercises is normal.
You can also try the following exercise movements:
- First, gently and slowly squeeze your pelvic floor muscles, lift, and hold for 5-8 seconds with normal breathing. Then, gently release and repeat the process 5-6 times. Take a break for up to 10 seconds between each movement.
- Attempt quick, strong, and short squeezes and repeat them up to 8 times.
Treating Pelvic Organ Prolapse With Vaginal Pessary
A vaginal pessary for pelvic organ prolapses is a flexible device that we place in the vagina to support the uterus and the pelvic organs.
These supportive devices come in different sizes and shapes. But we recommend that you consult a medical professional about choosing the right type and shape and have it fitted.
After the first insertion, you can get training to insert and remove the pessary yourself, as we do with tampons or contraceptive devices. But you must have a review regularly to check that everything is OK and as it should be down there.
These devices are most effective for uterine prolapse, but they may not be appropriate for everyone, and we wouldn’t recommend using a pessary in isolation. Instead, use them with pelvic floor exercises. Combined, they are an effective alternative to pelvic organ prolapse surgery.
Treating Pelvic Organ Prolapse With Surgery
Depending on your pelvic organ prolapse severity, surgical intervention might be required. This procedure is sometimes done via laparoscopic surgery.
The surgeon inserts a camera and surgical instruments through your navel to correctly reposition your uterus and other organs, reattaching them to supporting muscles and ligaments.
This type of surgery is the least invasive, but you may require an incision in the abdomen, which comes with a slightly longer recovery time. However, surgery isn’t a cure-all.
Symptoms can return if you don’t deal with the underlying cause of straining, coughing, constipation, or obesity. So it pays to find the root cause and strengthen the muscles with physical therapy first to avoid surgery.
How To Prevent Pelvic Organ Prolapse
If you keep in mind that the cause of pelvic organ prolapses is weak pelvic floor muscles, you can continually work on strengthening those muscles to avoid suffering from the condition. You can:
- Learn and practice pelvic floor exercises all through pregnancy
- Learn and do post-partum pelvic floor exercises after vaginal childbirth
- After menopause, use estrogen supplements (under medical supervision) and do pelvic floor exercises daily.
- In the case of obesity, try to decrease abdominal fat through a healthy diet and exercise.
- If you suffer from chronic constipation, try to incorporate plenty of green veggies, fiber, and fruit into your daily diet and drink 10-12 glasses of water because constipation can exacerbate your symptoms.
- Try not to strain when using the toilet to empty your bowels.


